Defibrillator technology has evolved significantly, improving both function and implantation methods. The combination of implanting an Extravascular Implantable Cardioverter Defibrillator (EV ICD) along with a CCM device is relatively new, though defibrillators have been in use for decades. The EV ICD was approved by FDA in October 2023.
When discussing these devices with patients, Dr. Chinmaya Mareddy, a Cardiac Electrophysiologists at the Centra Medical Group Stroobants Cardiovascular Center, begins by explaining various forms of cardiac implantable electronic device (CIED). CIED can be a pacemaker or a defibrillator. Pacemakers and defibrillators are both medical devices used to manage heart rhythm disorders, but they serve different purposes and functions.
Pacemaker helps to regulate a heart that beats too slowly. It sends small electrical impulses to the heart to maintain a regular rhythm and rate. Pacemakers can be single-chamber, dual-chamber, or biventricular, depending on the number of heart chambers they stimulate. They do not have the capacity to deliver high energy shocks.
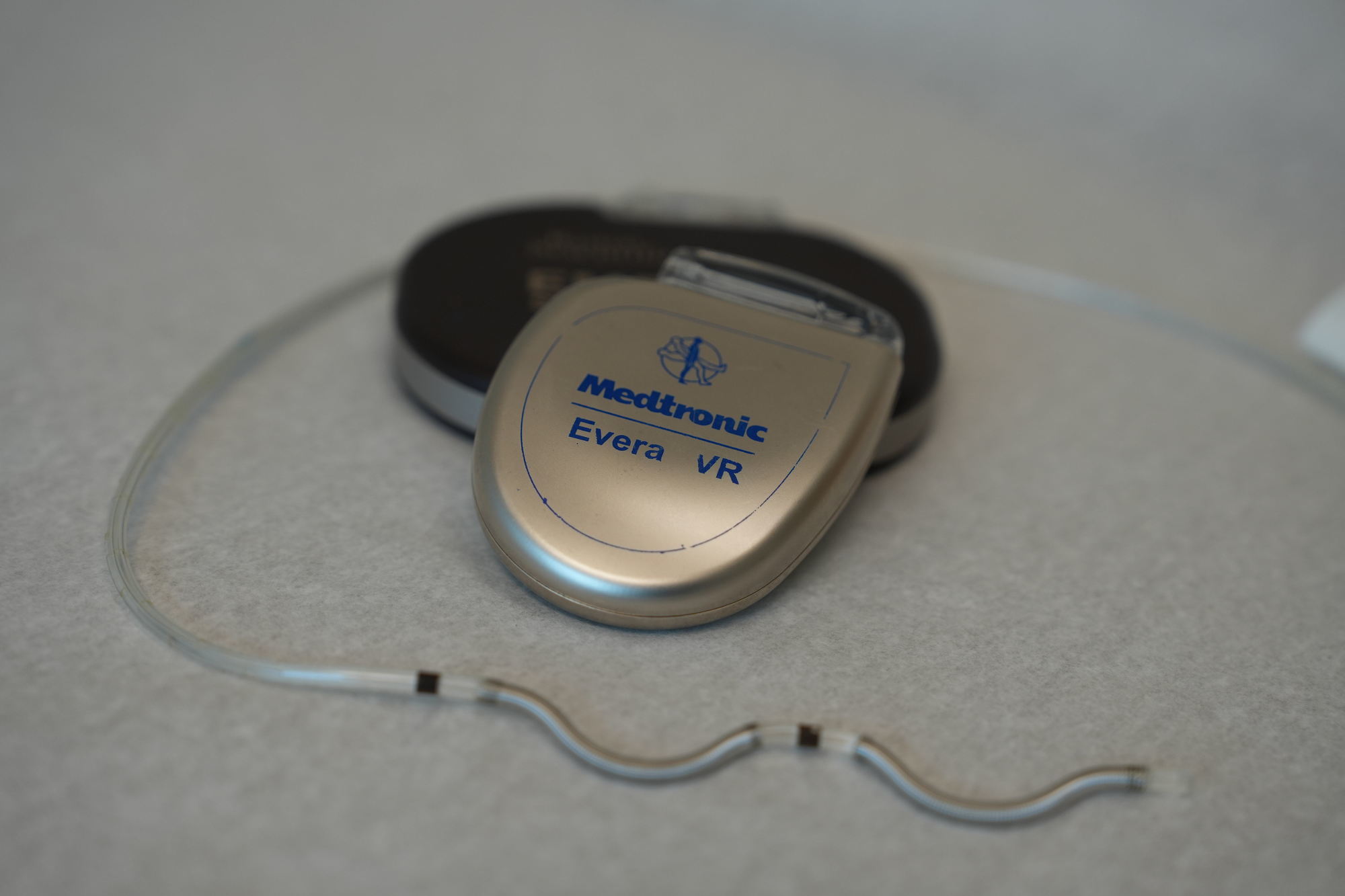
Defibrillator is designed to prevent or correct life-threatening arrhythmias, such as ventricular fibrillation or ventricular tachycardia, which can lead to sudden cardiac arrest. “It is like wearing a seatbelt” for patients who are at risk or had sudden cardiac arrest. It monitors the heart's rhythm and delivers a high-energy shock if it detects a dangerous arrhythmia. All defibrillators can work as a pacemaker as well if needed for a slow heart rate.
Implantable defibrillators come in two main forms:
- Transvenous ICD – This traditional type is implanted through a vein, placing leads inside the heart. It can function as both a pacemaker and a defibrillator. However, having leads in circulation for decades can pose risks, such as vein obstruction, infection, or bacteria adhering to the wires, sometimes necessitating device removal.
- Subcutaneous ICD – In use for over a decade, this type avoids placing leads inside the bloodstream. Instead, the wire is positioned under the skin, with the battery placed on the side of the chest. While it eliminates the risks associated with venous leads, it functions solely as a defibrillator and cannot provide pacing support.
A limitation of the subcutaneous ICD is that it only delivers a high-energy shock to correct life-threatening rhythms. However, we have learned that many of these dangerous arrhythmias, particularly ventricular tachycardia, can be stopped by painless anti-tachycardia pacing (ATP), which delivers small, rapid electrical impulses before resorting to a large shock.
This is where the EV ICD represents a breakthrough—it combines the benefits of a subcutaneous ICD with the ability to perform ATP. Approximately 70% of ventricular tachycardia episodes can be treated with these painless shocks, providing patients with a more comfortable and less traumatic experience. If ATP fails to correct the arrhythmia, the device will then deliver a high-energy shock as a backup measure.
The advantage of the EV ICD is that it offers the added protection of painless ATP without placing leads inside the bloodstream. This advancement provides a significant improvement in patient comfort and safety, reducing the risk of complications while maintaining effective life-saving capabilities.
Mareddy, together with Dr. Jose Silva, Dr. Houman Tavaf the team performed the first extraction of a transvenous ICD followed by the implantation of the new EV-ICD in Virginia in March 2024. Later that same year, Dr. Mareddy and his team performed a similar surgery followed by the implantation of a Cardiac Contractility Modulation (CCM) device to better meet the needs of a patient who had congestive heart failure. The combination of these devices used together made this the first patient in the world to be treated using this solution.
“Before we decided on this pairing procedure, we went through all the logistics behind the programming of the devices to see if it is feasible,” Dr. Mareddy said. “We spoke with both device companies when making the decision and came to the conclusion that we could work this out with very minimal things to keep in mind for specific cases.”
In one of the patients follow up appointments after the procedure significant improvement in heart failure symptoms were reported. Previously, the patient experienced shortness of breath during daily activities, but now feels much better in that regard. Other positive changes included a reduction in ventricular size, which may be contributing to her overall improvement.
While this combination of devices can be used for only a very targeted patient population, the team has already completed the pairing on a second patient with positive results.
“Here at Centra Cardiology and Cardiac Electrophysiology, Dr. Sackett has led the forefront of having the best technology to be available for patients,” Dr. Mareddy said. “I feel privileged to be part of this Heart & Vascular Institute Cardiac Electrophysiology team.”